Neurodegenerative brain diseases continue to pose a major medical challenge, with no known cure. Among them, Alzheimer’s disease is the most prevalent in older adults, affecting millions of people worldwide. It severely impairs daily functioning and places a significant burden on families and healthcare systems alike.
Although the exact cause of Alzheimer’s disease remains unclear, a prevalent scientific theory suggests that viral infections may play a significant role in its development. According to this theory, herpes simplex virus (HSV)—a common herpesvirus that typically causes cold sores, infects brain cells and may trigger inflammation and neuronal degeneration. Supporting evidence includes a strong correlation between HSV infection and Alzheimer’s disease, along with findings that antiviral treatments may reduce the risk of developing the disease. This theory is echoed by recent discoveries about Epstein-Barr virus (EBV)—another member of the herpes family, which has been found to play a significant role in the development of multiple sclerosis. Although HSV and EBV are distinct viruses associated with different neurodegenerative diseases, both cases reinforce the broader idea that latent viral infections may have substantial lasting effects on brain health.
HSV spends part of its time in an inactive state, known as the latent phase. During this phase, the virus remains dormant within the infected cells but can reactivate – beginning to replicate and spread to other cells in the body – when conditions become favorable. With over 70% of the global population already infected by HSV, this theory carries significant public health implications.
Another factor associated with the development of Alzheimer’s disease is a history of head injuries, particularly those caused by accidents or falls from a great height. While mild head injuries may cause temporary cognitive or motor impairments, more severe cases can result in irreversible damage. Studies have found that repeated head injuries can have long-term effects, and that the risk of dementia, particularly Alzheimer’s increases with the number and severity of head injuries.
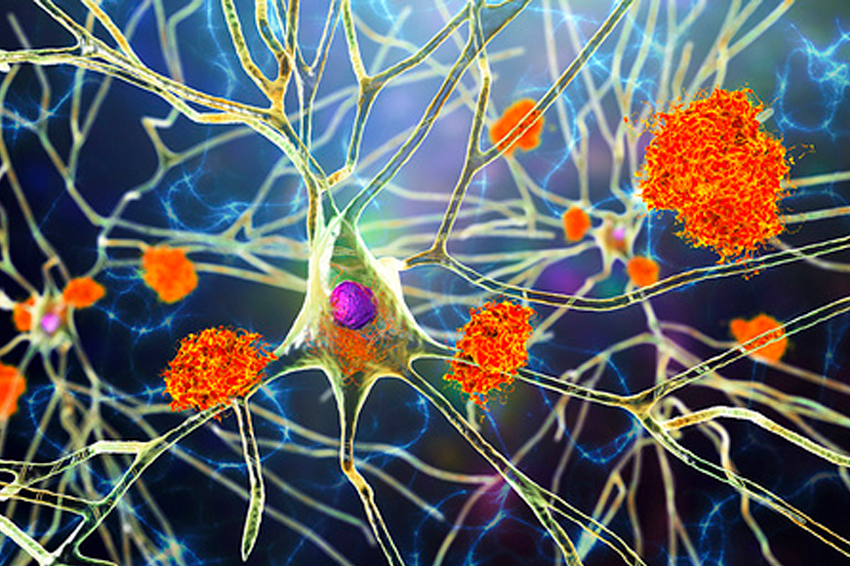
Alzheimer’s disease affects the functioning of many people worldwide. An illustration of neurons from an Alzheimer’s patient, showing amyloid beta protein deposits (in orange) | Kateryna Kon / Science Photo Library
Mini-Brains in the Lab
A recently published study explored the connection between head injuries and viral infections in the development of Alzheimer’s disease. The findings highlight how viruses can influence human health long after the initial infection. The researchers used a model of “organoids”—tiny three-dimensional structures composed of clusters of brain cells. They began by applying mechanical force to these artificial brains. Within a week, the organoids began to exhibit classic hallmarks of brain injury: the formation of an inflammatory response, the onset of gliosis (an overgrowth of glial cells that support and protect neurons), and even an excessive release of glutamate, a neurotransmitter critical for neuron-to-neuron communication. These results validated the model as an effective tool for studying brain injury and its underlying mechanisms.
The researchers then infected the organoids with HSV. Following the infection, they observed the buildup of amyloid beta protein deposits between brain cells between brain cells—one of the key hallmarks of Alzheimer’s disease. The experiment provided compelling evidence that, under laboratory conditions, HSV infection can accelerate processes associated with Alzheimer’s. The organoids also exhibited other well-known features of the disease, including the accumulation of phosphorylated tau protein, ongoing inflammation, and extensive gliosis. IRemarkably, the virus appeared to induce an Alzheimer’s-like state in a matter of days—even though in real-life cases, the disease develops over many years or even decades following HSV infection.

The researchers used a model of “organoids”—tiny three-dimensional structures made of brain cell clusters. Brain organoids in a glass container | Wikimedia, NIAID
The Dormant Virus Awakens
The researchers hypothesized that head injuries might reactivate a virus that had previously been dormant. To test this, they created a model of brain organoids infected with HSV in the latent phase. To test this, they developed a brain organoid model infected with HSV in its latent phase. The organoids were first infected with HSV and, after 24 hours, treated with the antiviral drug valacyclovir HCl (VCV) to inhibit viral replication and pushed the virus into its latent phase. The researchers then applied controlled mechanical injuries to the organoids and monitored cellular function, infection progression and viral reactivation.
As hypothesized, Alzheimer’s-like markers reappeared following the mechanical injury, and the previously dormant virus began to spread. Moreover, the researchers found that repetitive injuries, compared to single insults, resulted in a more pronounced Alzheimer’s disease-associated phenotype.These findings may help explain the high prevalence of Alzheimer’s disease among individuals with a history of head trauma, as well as the significant quantities of HSV found in their brains. They also underscore the importance of continued research into viral infections and their long-term impact on brain function and overall health.
It’s also important to note that complex interactions occur between different viruses, and in some cases, infection with one virus can trigger the reactivation of another. For example, infection with the coronavirus SARS-CoV-2 has been shown to lead to HSV reactivation. Thus, future treatments for neurodegenerative brain diseases may need to address viruses that are widespread in the general population. A deeper understanding of how our cells interact with infectious agents could ultimately pave the way for development of more effective therapies for chronic conditions.